Diagnosis
The diagnosis of malaria by blood tests is divided into microscopic and non-microscopic tests.
Microscopic Tests
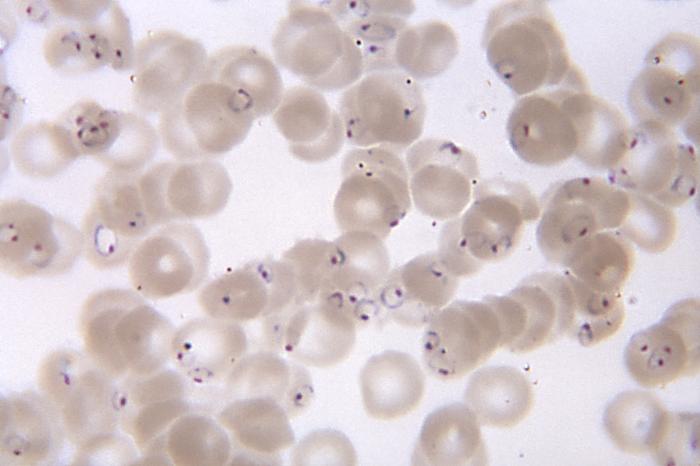
Direct microscopy is the most accepted method of diagnosing malaria. The tests involve staining and visualization of the protozoa under a microscope. The careful examination of a well-prepared and well-stained blood film currently remains the "gold standard" for malaria diagnosis.
1. Peripheral smear study
In peripheral smear study red blood cells are examined for intracellular malaria parasites after staining with Romanowsky on a blood smear. Thick blood smears are harder to interpret, but are more sensitive than thin smears thus have a higher yield. Thin smears allow identification of:
· Malaria species
· Quantify parasitaemia
· The presence of schizonts, gametocytes and malarial pigment in neutrophils and monocytes
The accuracy of the diagnosis depends on the quality of the blood smear and the experience of the laboratory personnel.
This images shows a blood smear seen under the microscope with the presence of numerous P. falciparum rings form parasites.
|
Image courtesy of https://commons.wikimedia.org/wiki/File:Plasmodium_falciparum_rings_form_parasites4885_lores.jpg Images is in the public domain and thus free from copyright restrictions |
2. Quantitative Buffy Coat (QBC) test
A novel method for identifying a malaria parasite in peripheral blood is the QBC test. The main idea in QBC is centrifugation; centrifuged red blood cells are stained with acridine and examined under UV light. Red cells containing the protozoa are:
· less dense than normal
· concentrate just below the leukocytes
· concentrate at the top of the erythrocyte column
QBC is a fast, but less accurate.
Non-microscopic Tests
These tests have removed the dependence of malaria diagnosis on the microscope.
Rapid antigen detection tests
Detect species-specific circulating parasite antigens. Tests based on polymerase chain reaction for species-specific Plasmodium genome are more sensitive and specific than are other tests, detecting as few as 10 parasites/μl blood. However, Antibody detection has no value in the diagnosis of acute malaria and is mainly used for epidemiologic studies. They are easy to perform and do not require trained laboratory personnel nor special equipment. In addition, not all species of plasmodium can be diagnosed- P. falciparum can but not the others.
Most importantly
1. A negative test DOES NOT rule out malaria. Repeated tests may have to be done in all doubtful cases depending on
· Duration of the illness
· level of parasitaemia
· expertise of the technician
· method of examination
2. Parasitaemia is very common in endemic areas. The presence of the parasite should not lead to a conclusion that the parasite is what is causing the patients symptoms therefore further diagnostic test must be carried out including lumbar puncture to remove the bacterial infection.